Details About
Shoulder Arthroscopy
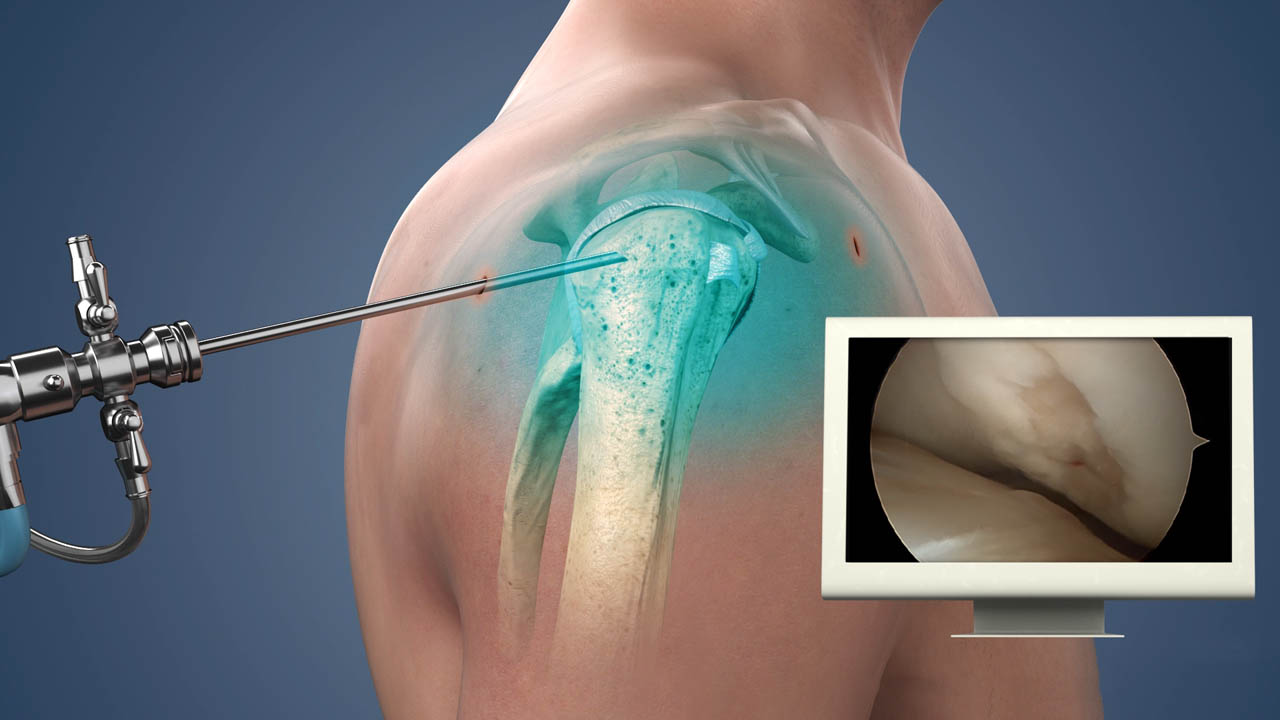
Visualizing and Restoring Shoulder Health
Shoulder arthroscopy, a cutting-edge minimally invasive surgical technique, offers both diagnostic clarity and therapeutic possibilities for a range of shoulder joint concerns. In this procedure, a skilled orthopedic surgeon employs a slender, fiber-optic camera called an arthroscope to gain a comprehensive view of the shoulder's internal structures without the need for extensive incisions. This enables precise assessment and diagnosis of conditions such as rotator cuff tears, labral injuries, or inflammation. Additionally, arthroscopy allows for targeted interventions through tiny incisions, including procedures like repairing the rotator cuff, addressing labral tears, or removing loose fragments. The minimally invasive nature of shoulder arthroscopy often translates to shorter recovery times, reduced pain, and minimized scarring compared to traditional open surgeries. As a result, shoulder arthroscopy has emerged as a versatile tool in modern orthopedics, offering patients an expedited path to both accurate diagnosis and effective treatment for various shoulder-related ailments.
Shoulder arthroscopy, often referred to as shoulder scope, is a minimally invasive surgical procedure employed for both diagnosis and treatment of various shoulder joint ailments. This technique utilizes a specialized instrument known as an arthroscope, equipped with a camera and a light source, to gain a clear view of the interior of the shoulder joint. By inserting this tiny, flexible device through small incisions in the shoulder, orthopedic surgeons can investigate the joint's condition and perform surgical interventions as necessary. Shoulder arthroscopy is a versatile procedure commonly used to address a range of issues affecting the shoulder, such as rotator cuff tears, labral injuries, bursitis, and more.
One primary purpose of shoulder arthroscopy is to provide an accurate diagnosis for unexplained shoulder pain or discomfort. This minimally invasive approach enables surgeons to visually inspect the joint's structures and pinpoint the root cause of the patient's symptoms. Additionally, shoulder arthroscopy is a valuable tool for therapeutic purposes. Surgeons can perform various procedures during the arthroscopy, including repairing the rotator cuff, addressing labral injuries, removing inflamed bursa, and excising problematic tissue. This minimally invasive approach often leads to quicker recovery times compared to traditional open surgery.
Post-surgery, patients typically experience a faster and smoother recovery compared to more invasive procedures. They may be discharged on the same day or require only a brief hospital stay, depending on the complexity of the surgery. Recovery times can vary based on the specific procedure performed, but many patients can expect to resume their normal activities within a few weeks to a few months. Physical therapy is often recommended as part of the rehabilitation process, aiding patients in regaining strength and mobility. While shoulder arthroscopy is generally considered safe, potential risks and complications should be discussed with the surgeon before the procedure. Overall, shoulder arthroscopy is a valuable and widely used technique for diagnosing and treating a range of shoulder joint conditions, offering patients a less invasive and faster path to relief and recovery.
1. Diagnosis
Armed with these invaluable insights, orthopedic specialists are adept at offering precise diagnoses, which subsequently inform targeted treatment strategies tailored to alleviate pain and restore the shoulder's functionality. For individuals grappling with the uncertainty of unexplained shoulder discomfort, shoulder arthroscopy represents a beacon of hope. Its minimally invasive nature translates to reduced post-operative discomfort, expediting the path to recovery. Patients often experience a swifter return to their daily routines, underscoring the procedure's effectiveness as a diagnostic and therapeutic approach. Shoulder arthroscopy stands as an exemplary illustration of the marriage between medical innovation and patient-centric care within the orthopedic field.
In addition to the clinical evaluation, diagnostic imaging studies such as X-rays and MRIs are often performed. X-rays provide detailed images of the shoulder joint, allowing the surgeon to assess the extent of joint degeneration, bone damage, and alignment issues. MRIs offer a more comprehensive view of the soft tissues surrounding the shoulder joint, helping to identify conditions like labral injuries or rotator cuff tears. Collectively, this comprehensive evaluation guides the surgeon in making an informed decision regarding the necessity and appropriateness of shoulder arthroscopy for the patient, taking into account their overall health and the severity of shoulder joint issues.
In summary, shoulder arthroscopy emerges as a powerful diagnostic ally in the realm of orthopedic medicine, shedding light on the origins of enigmatic shoulder pain. This minimally invasive procedure, facilitated by the arthroscope's advanced capabilities, delves deep into the intricacies of the shoulder joint. It effectively detects an array of issues, from rotator cuff tears to labral injuries, aiding orthopedic specialists in formulating precise diagnoses and tailored treatment plans. The patient-friendly nature of this approach ensures a smoother post-operative experience, accelerating the recovery process. In the ever-advancing landscape of medical technology, shoulder arthroscopy signifies a significant leap forward, putting patients on the fast track to relief and functional restoration.
2. Treatment
In addition to diagnosing shoulder problems, arthroscopy allows for minimally invasive treatment. Some of the most common procedures performed during shoulder arthroscopy include:
1. Rotator Cuff Repair
Indication
Rotator cuff injuries are common and can cause shoulder pain and reduced range of motion. Repairing the rotator cuff during arthroscopy can help alleviate these symptoms.
Procedure
The surgeon uses arthroscopic tools to access the torn rotator cuff. The torn tendons are reattached to the bone using sutures or anchors to restore the function of the rotator cuff.
2. Labral Repair
Indication
Labral tears or injuries to the cartilage ring surrounding the shoulder socket can lead to instability and pain in the shoulder joint.
Procedure
The surgeon uses arthroscopic instruments to access the labral tear and repair it. This can restore stability to the shoulder joint and reduce pain.
3. Bursa Removal
Indication
Inflammation of the bursa sac in the shoulder can cause pain and limited mobility. Removing the inflamed bursa can relieve these symptoms.
Procedure
Arthroscopic tools are used to remove the inflamed bursa, reducing pain and improving shoulder function.
4. Removal of Loose Bodies
Indication
Small fragments of bone or cartilage, known as loose bodies, can interfere with joint movement and cause pain in the shoulder.
Procedure
The surgeon uses arthroscopic tools to locate and remove these loose fragments. This helps restore normal joint function.
5. Synovectomy
Indication
A synovectomy is done when the synovial membrane, which lines the inside of the joint, becomes inflamed and painful, often seen in conditions like rheumatoid arthritis.
Procedure
The surgeon uses arthroscopic instruments to remove inflamed synovial tissue. This helps reduce pain and swelling associated with the inflamed synovium.
NOTE:
Each of these procedures is tailored to the specific condition and needs of the patient. The choice of procedure and the approach used depend on the surgeon's assessment during the arthroscopic examination and the severity of the shoulder problem. It's important to consult with a qualified orthopedic surgeon to determine the most suitable treatment for your individual situation.
3. Recovery After Shoulder Arthroscopy
Shoulder arthroscopy, being minimally invasive compared to traditional open surgery, offers several advantages in terms of recovery. Patients typically go home on the same day of the procedure or after a short hospital stay, depending on the complexity of the surgery.
Recovery times can vary based on the specific procedure performed. However, most patients can expect to return to their normal activities within a few weeks to a few months. The minimally invasive nature of shoulder arthroscopy often results in reduced post-operative discomfort, expediting the path to recovery.
To aid in rehabilitation and regain strength and mobility, physical therapy is often recommended as a crucial component of the recovery process. Physical therapists work with patients to implement targeted exercises and activities that facilitate the healing of the shoulder joint and improve overall function.
The post-operative care plan may include specific instructions for wound care, pain management, and gradual resumption of activities. Patients are typically encouraged to follow a structured rehabilitation program, which may involve a combination of in-person physical therapy sessions and home exercises.
Monitoring progress through follow-up appointments with the orthopedic surgeon is important. These appointments allow for the assessment of healing, the adjustment of the rehabilitation plan as needed, and addressing any concerns or questions the patient may have.
In summary, the recovery process after shoulder arthroscopy involves a comprehensive approach, encompassing post-operative care, physical therapy, and ongoing monitoring. The patient's commitment to following the prescribed rehabilitation plan significantly contributes to the success of the procedure in alleviating pain and restoring shoulder function.
4. Risks of Shoulder Arthroscopy
Shoulder arthroscopy is generally considered a safe procedure, thanks to its minimally invasive nature. However, like any surgical intervention, it does come with potential risks and complications that patients should be aware of.
1. Infection: Infection is a risk associated with any surgical procedure. The use of arthroscopic instruments and techniques minimizes the risk, but it's essential to follow post-operative care instructions to reduce the chances of infection. Signs of infection, such as increased pain, redness, or fever, should be promptly reported to the healthcare provider.
2. Bleeding: While the risk of significant bleeding during shoulder arthroscopy is low, it's not entirely eliminated. The surgeon takes precautions to minimize bleeding during the procedure, but some oozing may occur. Patients are usually monitored post-surgery to ensure bleeding remains within acceptable limits.
3. Blood Clots: The formation of blood clots, known as deep vein thrombosis (DVT), is a potential risk following any surgery. Patients are often encouraged to move their arms and engage in specific exercises to prevent DVT. In some cases, blood-thinning medications may be prescribed to reduce the risk.
4. Damage to Surrounding Tissues: During shoulder arthroscopy, there is a slight risk of unintentional damage to surrounding tissues, such as nerves, blood vessels, or adjacent cartilage. Surgeons take great care to avoid such complications, and the use of arthroscopic visualization aids in precision.
5. Outcomes of Shoulder Arthroscopy
The success of shoulder arthroscopy is influenced by the specific condition being treated and the surgeon's skill. For many patients, this procedure provides significant relief from pain and improved shoulder function. It is especially effective in cases involving common issues like rotator cuff tears or labral injuries.
1. Procedure Success: The success of shoulder arthroscopy depends on the specific condition being treated. Many patients experience significant relief from pain and improved shoulder function after arthroscopy. However, outcomes can vary from patient to patient.
2. Variability in Outcomes: It's important to note that outcomes can vary based on the severity of the condition, individual healing responses, and adherence to rehabilitation protocols. The extent of improvement may differ among patients.
3. Additional Treatment: In some instances, shoulder arthroscopy may be part of a broader treatment plan. Patients with extensive ligament damage or complex conditions may require additional surgical procedures, long-term rehabilitation, or additional treatments to achieve optimal outcomes.
4. Postoperative Rehabilitation: The effectiveness of shoulder arthroscopy is enhanced when patients actively participate in postoperative rehabilitation. Physical therapy, exercises, and lifestyle modifications prescribed by the healthcare team can significantly impact recovery and long-term success.
5. Consultation with Surgeon: To better understand potential outcomes and address specific concerns, patients are encouraged to engage in thorough discussions with their orthopedic surgeon before the procedure. This dialogue allows for realistic expectations and informed decision-making regarding the course of treatment and expected results.



